A nursing assessment form is a document filled out by the nurse when she is performing nursing assessments that includes height and weight measurements, temperature, blood pressure, heart and respiratory rate.
Table of Contents
- 1 What is a nursing assessment form?
- 2 Why does a nursing assessment important?
- 3 What to include in a nursing assessment form?
- 4 The uses of nursing assessment form:
- 5 How to write a nursing assessment?
- 6 How a nursing assessment form is different from a physical assessment?
- 7 Conclusion:
- 8 Faqs (Frequently Asked Questions)
What is a nursing assessment form?
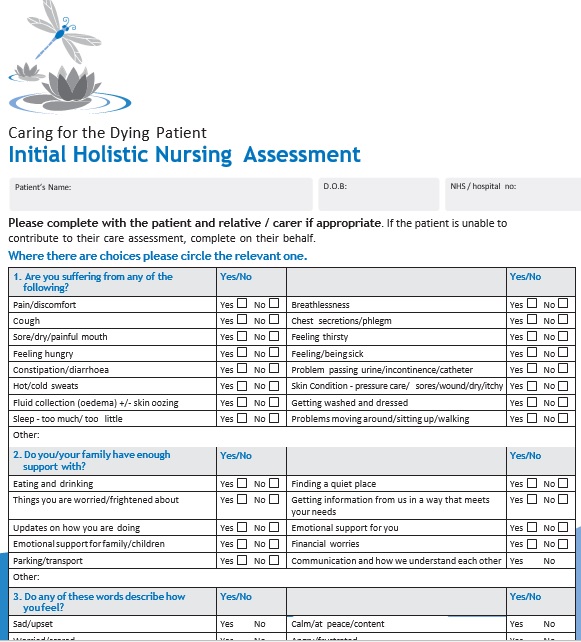
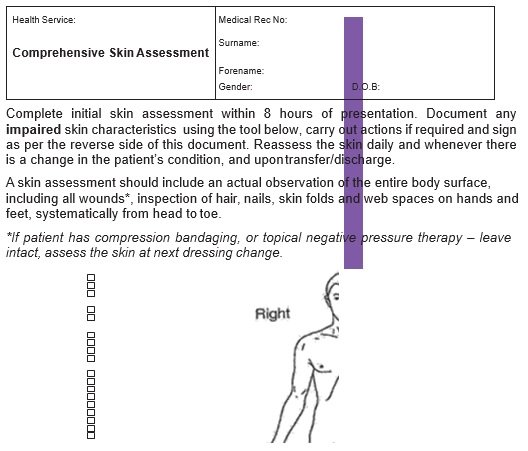
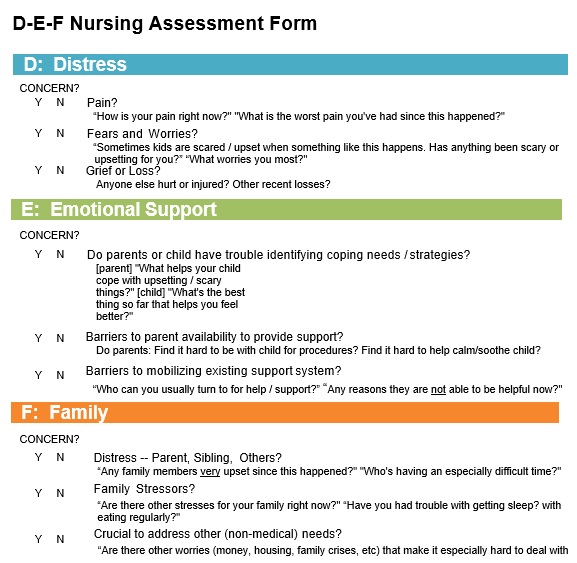
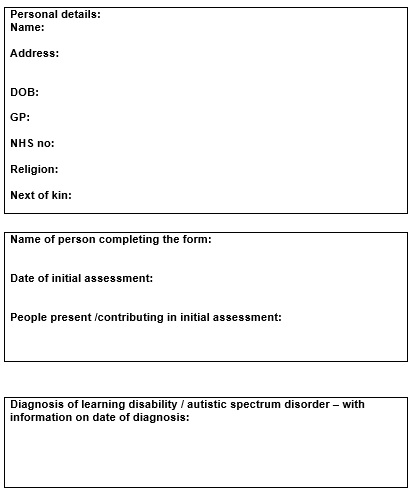
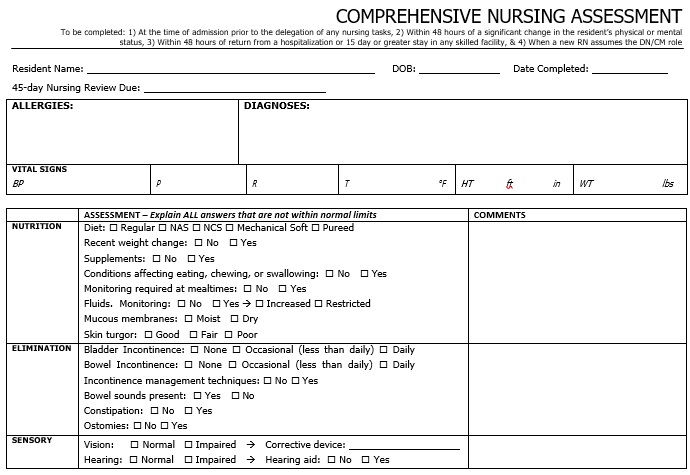
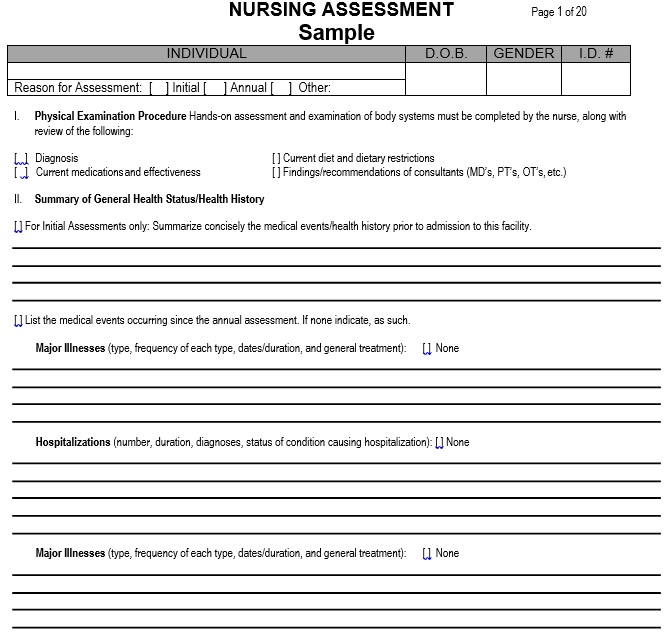
A nursing assessment form includes information regarding the physiological, psychological, spiritual, and sociological status of a patient. In the nursing process, the assessment is the first step. You can use nursing skin assessment forms to determine the current and future needs of a patient. Before you can properly evaluate an individual, you should go through certain set procedures.
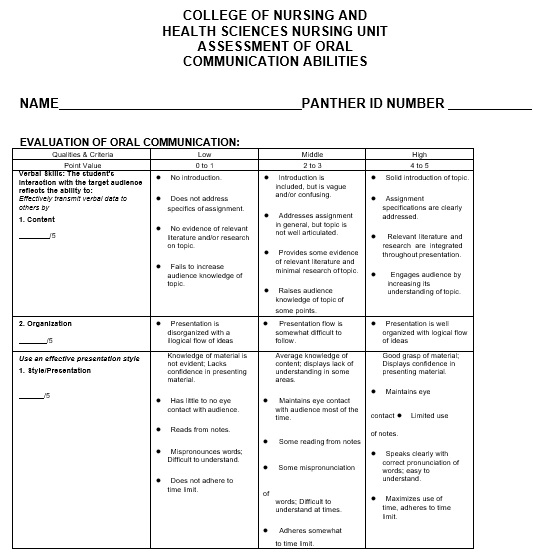
Typically, when conducting these evaluations, you will use a nursing assessment sheet that you will fill up. A nursing assessment is basically an organized set of processes used to give optimal care for your patients. This assessment has a wide scope as it pays attention on the whole body system. Here are the different types that pay attention to the specific parts of the assessment;
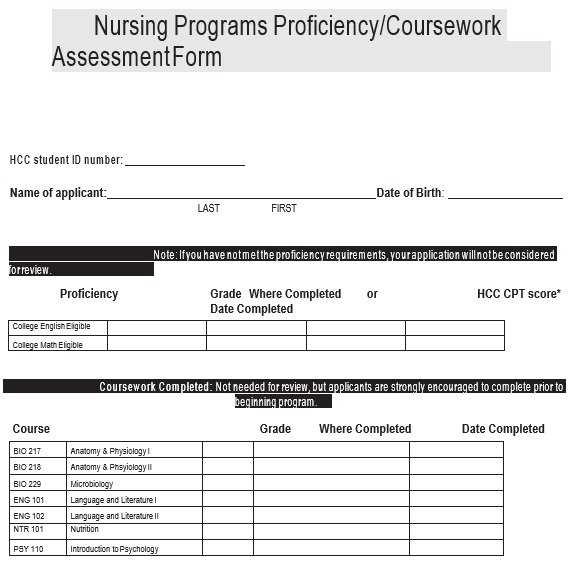
- Learning needs: In this type, determine deficiencies in the knowledge that acts as the basis of the learning requiring of a person that you can identify.
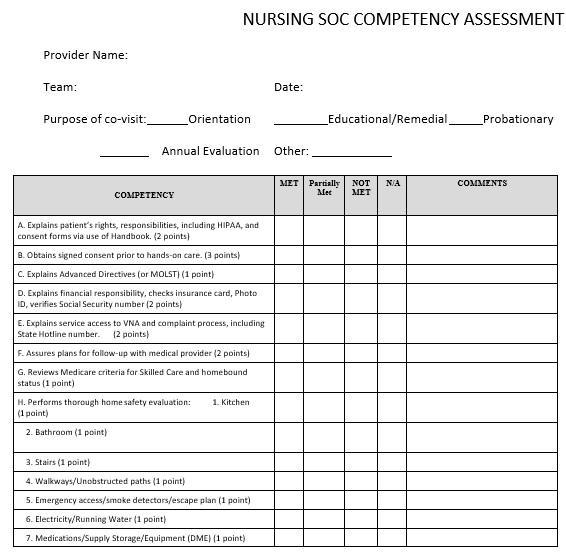
- Competency: This is the continuous evaluation of the knowledge, skills, and development of an individual that makes them able to perform activities.
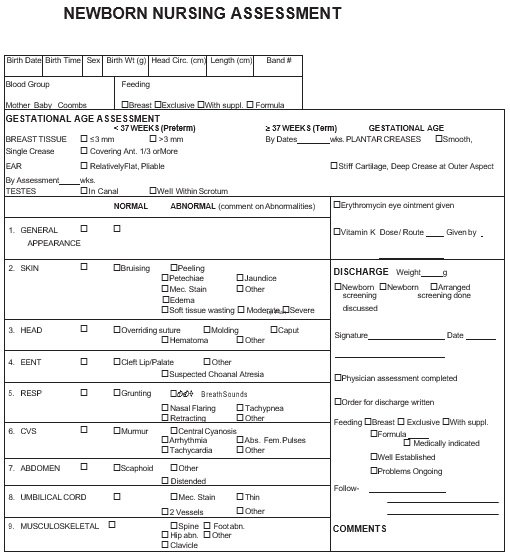
- Physical: This is an entire head-to-toe assessment of a patient.
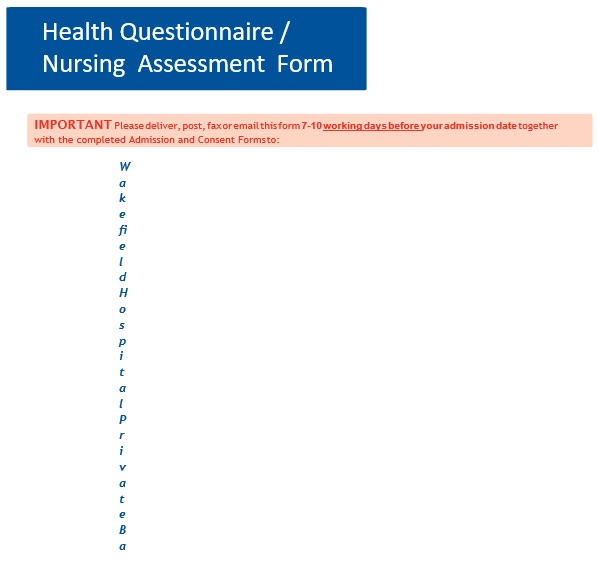
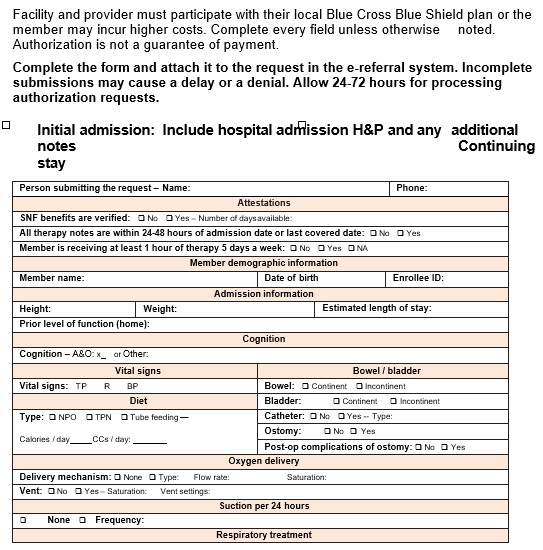
- Admission: They should go through physical assessments and statistics before a patient gets confined in a hospital. This acts as a baseline for the needed actions you have to take and for the patient records.
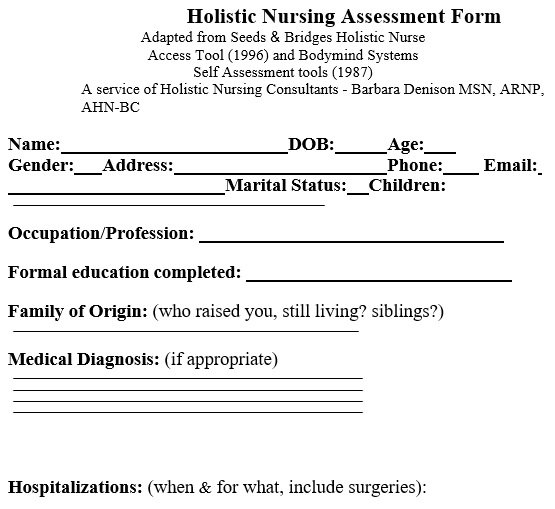
- Holistic: This involves sociological, cultural, spiritual, and psychological requirements. You derive your nursing implementations from the details you collect from your patient.
Why does a nursing assessment important?
In the development of a plan to deliver the best possible patient care, nurses know that a comprehensive nursing assessment is an essential first step. A nursing assessment form is a key part of nurse responsibilities and roles. It is an important tool to learn about a patient’s symptoms, overall health, and concerns.
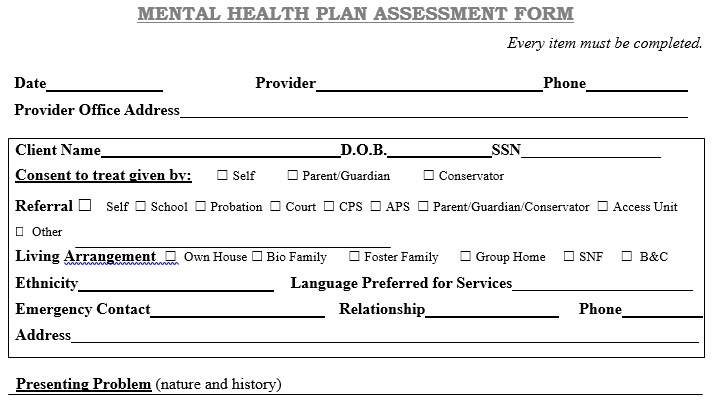
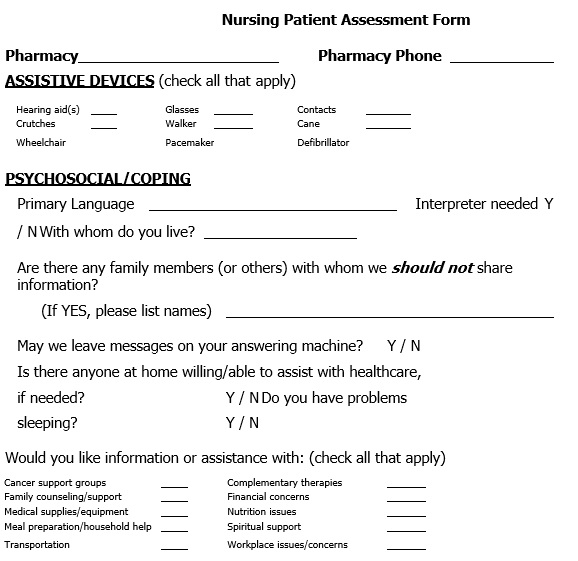
In addition, a nursing assessment template is an important factor. This is because it is a place where you gather comprehensive data to help in the determination of your diagnoses. This data then you can use to establish nursing care plans to help improve health outcomes. The comprehensive data on these forms includes the following;
- Psychological
- Socioeconomic
- Social
- Information of health, lifestyle, and spiritual physiological determinants
The comprehensive health assessment has several elements. You must develop a rapport with your patients before the assessment begins. In this rapport, you should first introduce yourself then describe what you will do during the assessment and why.
You have to put the patients as ease while conducting these assessments and establishing a rapport as patients become anxious. However, with the healthy history of the patient, most comprehensive nursing assessments begin. This includes information about their past injuries or illnesses that includes the following;
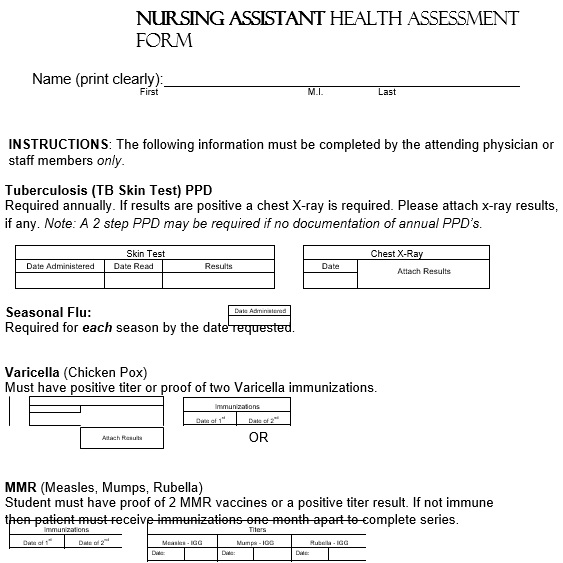
- Childhood immunizations and illnesses
- Surgeries
- Hospitalizations
- Allergies
- Chronic illnesses
- The illnesses that are inherited from their family
The healthy history of the patient is one of the components of a nursing assessment. Before you forward the process to the physical examination, you will ask a patient to describe here the;
- The symptoms they feel
- When their symptoms began
- How they developed
Physical examination is also an important component. It begins with a complete set of vital signs such as blood pressure, respiratory rate, temperature, and heart rate. It is important to learn how to keep up with distinct patient characteristics due to the increasing rate of chronic conditions and the growing elderly population.
What to include in a nursing assessment form?
In terms of structure and general areas of information, there are various things to include in a nursing assessment form. Let us discuss below the main areas of it;
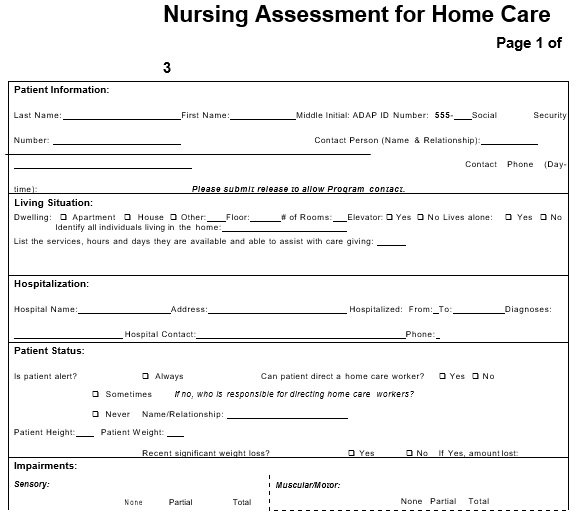
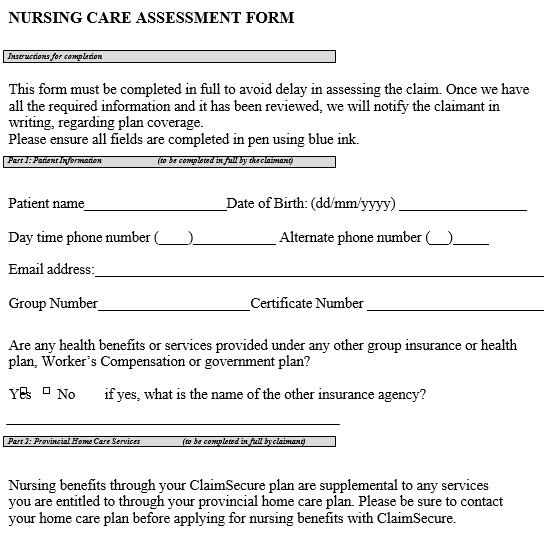
Patient information
Usually, the nurse assessment form has a section for basic patient details such as name, address, contact details, and occupation.
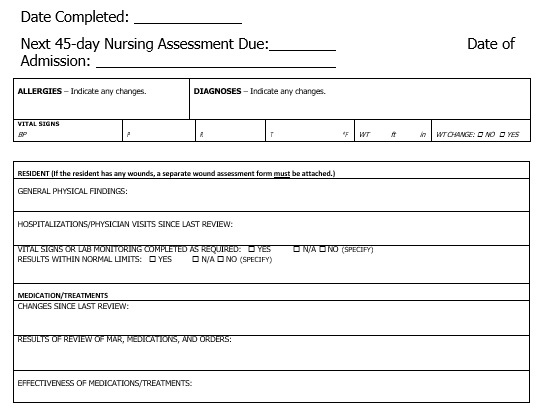
Patient evaluation
The patient evaluation area may has a section for the following;
- Measurements of vital signs
- Personal details like height, weight, etc.
- Any existing medical conditions or allergies
- Details regarding current medical complaints and symptoms
Patient medical history
It consists of sections for past conditions and any common family illnesses.
Nurse signature
There must be a section for the nurse details and signature who is conducting the assessment.
The uses of nursing assessment form:
A nursing assessment form is basically used to collect details regarding new and existing patients. It is collected to determine any current, ongoing, or potential care requirements. They make medical organizations able to gather detail in a standardized manner. Thus, healthcare professionals become able to administer treatment and record patient health efficiently. Organizations can save significant amounts of resources and employee time if they use nursing assessment form on daily basis. They can streamline their workflow by using a template.
How to write a nursing assessment?
You should include the following while making the nursing assessment form;
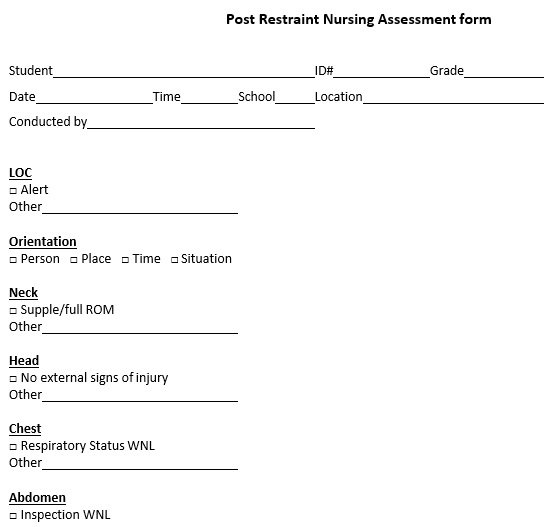
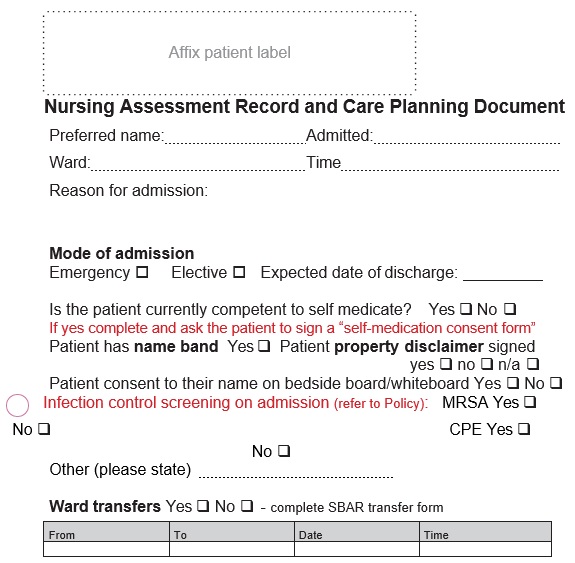
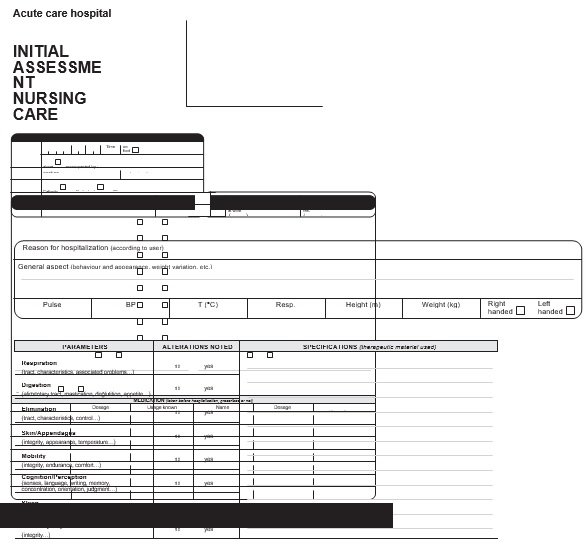
Admission Assessment
Admission assessment should be completed within 24 hours of the patient’s admission. You should complete it with the patient, a caregiver, or a parent upon the patient’s arrival. Then, into the progress notes of the patient, and enter any additional information.
Patient history
You as a nurse have to discuss the following with your patient;
- the patient’s current illness or injury history
- other related details regarding patient’s past history
- any allergies or identical reactions
- any medications that the patient is taken currently
- immunization status
- implants, social, and family history
Furthermore, you can also discuss any overseas travel. You should conduct patients’ overall emotional, behavioral, and physical assessment upon their admission. After that, continue to analyze them throughout their stay in the hospital.
Vital Signs
On your patient’s observation flowsheet, this includes recording baseline observations. This is an essential aspect of admission documentation and evaluation. You have to accomplish an ongoing assessment of vital signs as mentioned for your patient. Moreover, every two hours or as your patient’s condition requires, you should review the VICTOR graph. This enables you to analyze any trending of essential signs that may support your clinical assessment process.
Physical Assessment
You should conduct a structured physical examination of your patient. This can help you get a complete assessment of your patient. Some techniques such as inspection or observation, percussion, auscultation, and palpation are used to obtain this information. Use your clinical judgment in order to make a decision on the extent of the assessment required. Here is a few assessment information that includes;
- Primary assessment
- Shift assessment
- Focused assessment
- Neurological system
- Respiratory system
- Gastrointestinal
- Musculoskeletal
- Skin
- Eye
- ENT (ear, nose, throat
Assessment Evaluation
In the end, before going to the evaluation phase of your assessment, you should ensure that the information you collect is properly documented, complete, and accurate. In making clinical decisions and the plan of care for the patient you’re assessing, you should use problem-solving and critical thinking skills.
How a nursing assessment form is different from a physical assessment?
Physical assessment is performed by the nurses in which they monitor important signs such as pulse rate and blood pressure and record them in a nursing assessment form.
On the other hand, the nurse assessment form is also used to record the following information;
- Medical history
- Habits and lifestyle choices
- Close family members long-term health conditions
- Current treatment or medication plans
- Current symptoms
- Results of a health examination
- Results of any lab tests which is performed before the assessment
Conclusion:
In conclusion, a nursing assessment template is used by a nurse while assessing the patient. This document makes sure accurate, safe, and effective nursing care. Nursing assessment involves the psychological, physical, social, and spiritual aspects of a patient. It also provides you a better understanding of the needs and wants of a patient.
Faqs (Frequently Asked Questions)
The nursing process makes sure a high-quality patient care and consists of five phases;
1- The first phase: it is the assessment phase which contains patient’s information.
2- The second phase: diagnosis is conducted in relation to patient’s signs and symptoms in this phase.
3- The third phase: it has a plan for the patient’s care.
4- The fourth phase: in this phase, the nurse’s plan of action is implemented.
5- The last phase: this phase is the assessment of the entire patient care from the nurse.