A progress note template is used by healthcare professionals to record the details of the clinical status of a patient. This helps the doctors to reassess the data and recovery graph of the patient.
There are different formats of progress note templates available. However, the detail present on the progress note depends on the details in hand and the important information to record.
Using progress note templates, the physicians record the information about patients’ health status and use it to compare with the past status. So, the best plans for the treatment can be made based on the findings of this comparison. Therefore, these notes are written at a regular interval during a patient is hospitalized.
Progress note template is really helpful as it acts to provide medical facts in the best communication media about the medical condition of any patient for medical experts.
Most of the hospital records include progress notes of the patients as proof of the best care has been provided to the patients based on the diagnosis. Therefore, the use of progress note templates helps to develop a proper system to manage the progress notes. Moreover, an easier-to-understand, effective, and accurate progress note can be created using the template.
The progress note template allows recording complete information of every encounter with the transparency and accountability of the material.
Table of Contents
- 1 What is the Progress Note?
- 2 What do you know about Process Notes in Counseling?
- 3 Types of Progress Note Template
- 4 The purpose of progress notes:
- 5 Elements of Progress Note Template
- 6 How Should I Write a Progress Note?
- 7 How can I write a Good Patient Note?
- 8 How to create effective progress notes by using the SOAP format?
- 9 How can you differentiate between SOAP notes and progress notes?
- 10 How can you differentiate between progress notes and psychotherapy notes?
- 11 Do’s and Don’ts of Progress Note Template
- 12 Faqs (Frequently Asked Questions)
What is the Progress Note?
A progress note is a part of a medical record that keeps the ongoing record of the patient’s illness and treatment. During the course of hospitalization or over the course of outpatient care, physicians or health care professionals record details to a document concerning the progress or lack of progress made by patients. For the patients who are not critical, a progress note may be written daily. And, for critical patients, the note has written hourly. It should be written clearly, the date and time recorded, and the note signed.
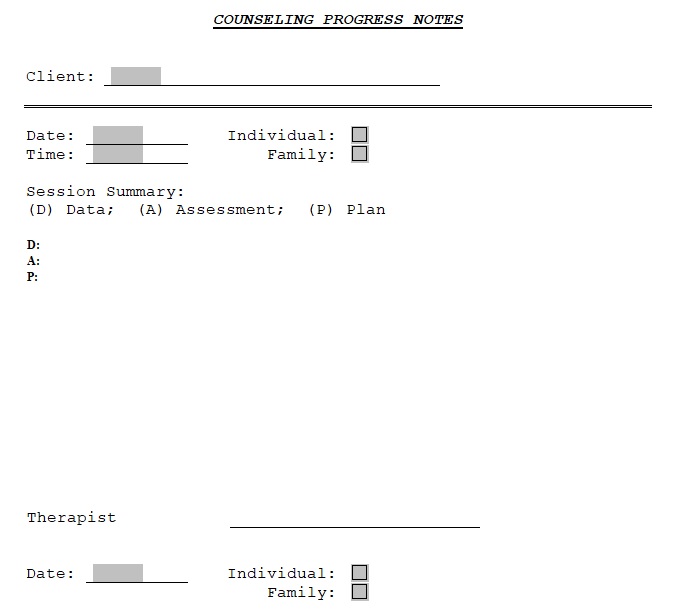
What do you know about Process Notes in Counseling?
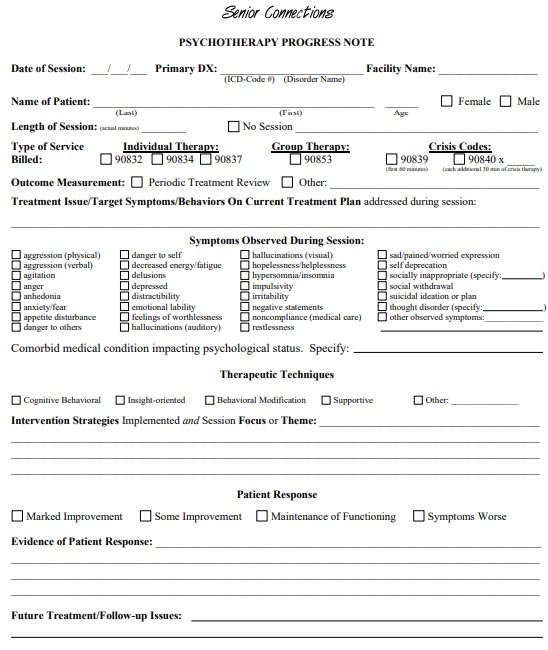
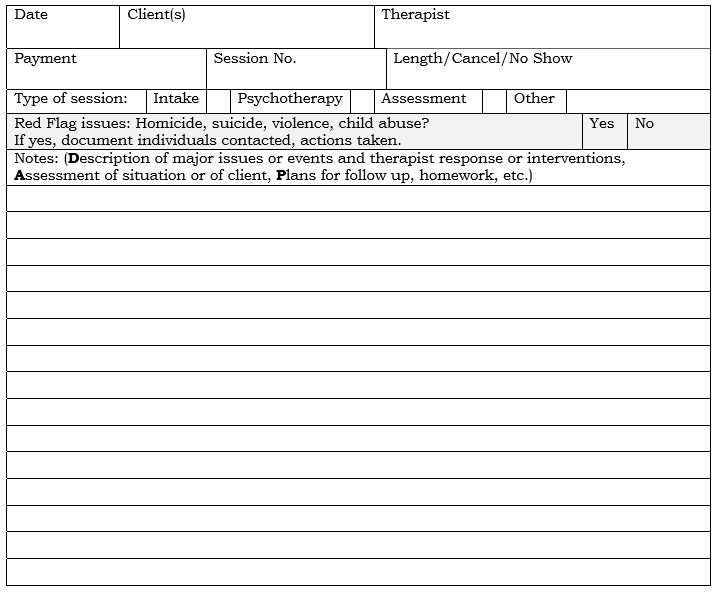
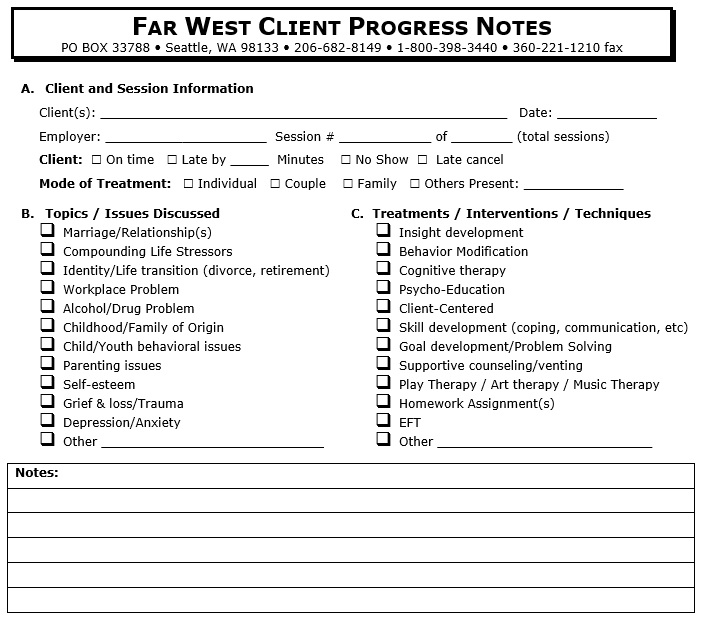
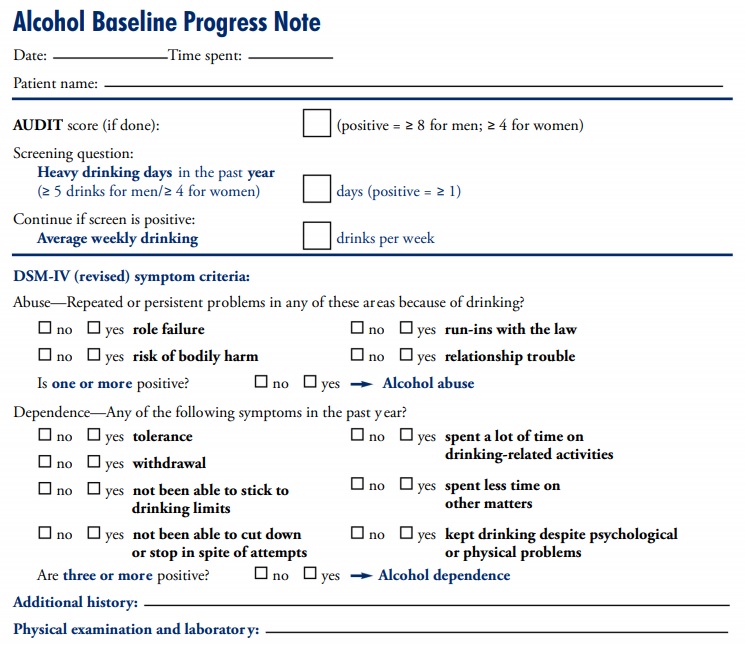
Process notes in counseling are also known as psychotherapy notes or private notes, taken by the mental health professionals or physicians for documenting or analyzing the content of conversation during a therapy session. It involves hypotheses, observations, thoughts, and further questions that a professional may have about the patient. These notes act as a reference point for the mental health professionals concerning the patient’s diagnosis and progress.
Types of Progress Note Template
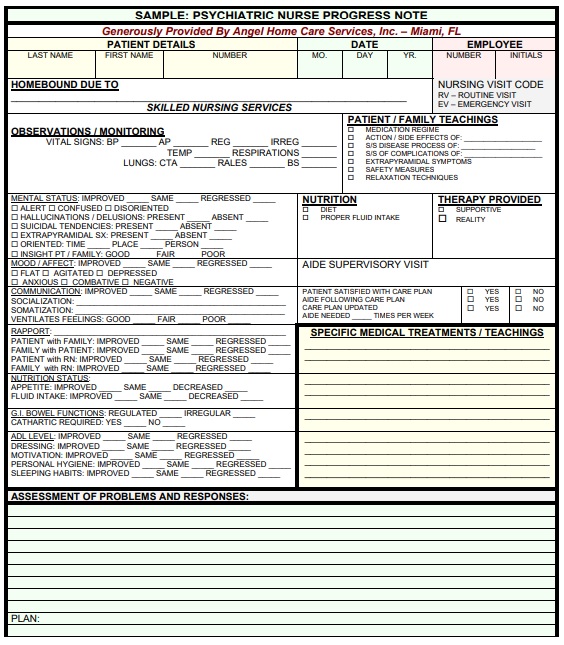
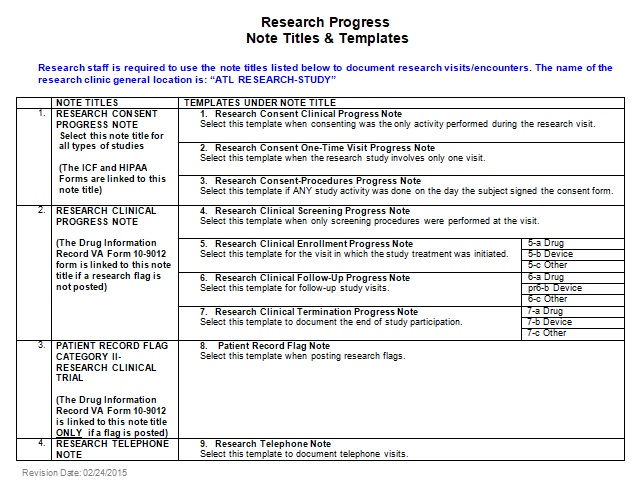
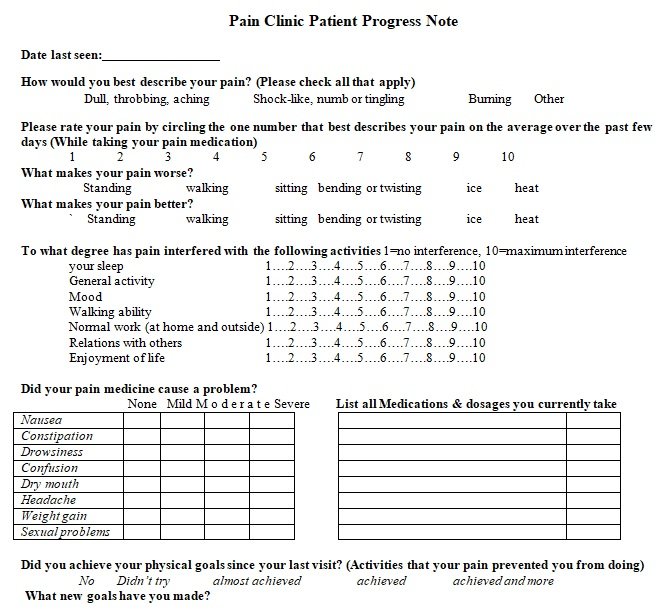
There are different types of progress note templates used by medical physicians and nurses. It depends on the information available and necessary to record. Moreover, the most common types of progress note templates are the SOAP note template and the DART system template.
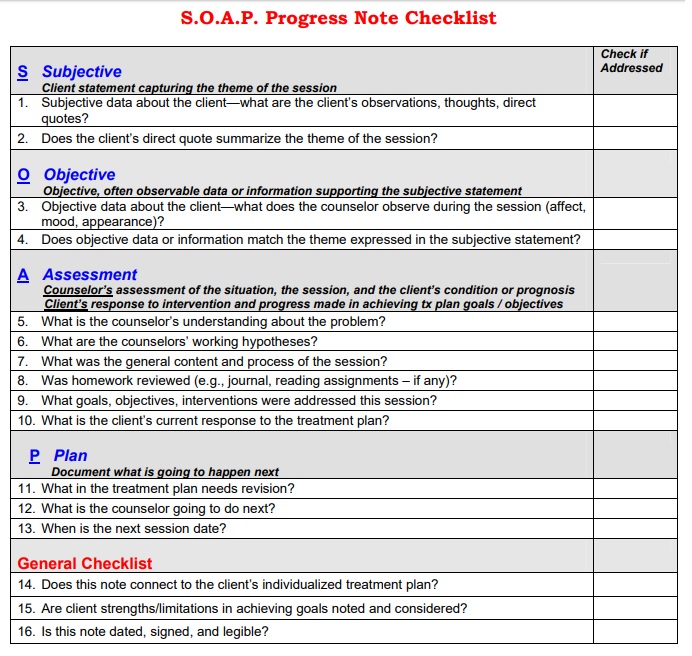
The SOAP stands for Subjective, Objective, Assessment, and Plan. What the patient share with the doctor is known as subjective. While the objective is determined by physical examination, and lab tests. Moreover, the assessment is the diagnosis provided by the doctor to plan the treatment accordingly.
Another type of progress note template is the DART system. It stands for Description, Assessment, Response, and Treatment. The proper documentation of the diagnosis, examination, and treatment is a very important part of the process.
The purpose of progress notes:
Here are a few purposes for making progress notes;
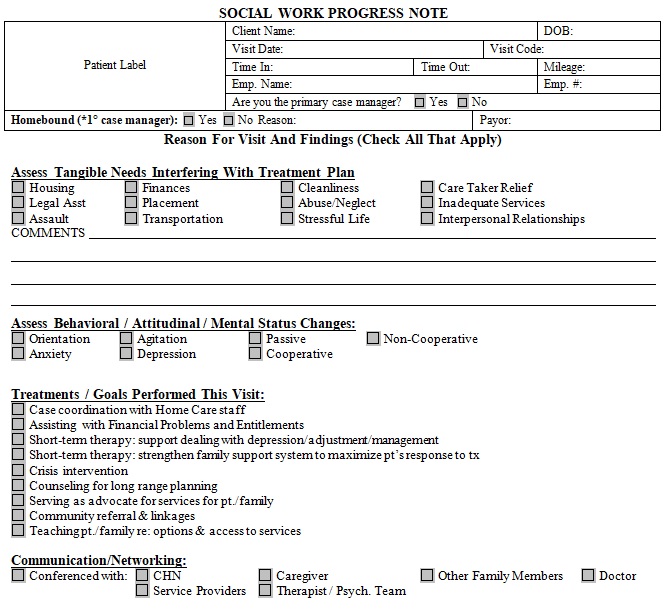
- Facilitating patient care
- Having a medical-legal document
- Help in billing
- Performing research
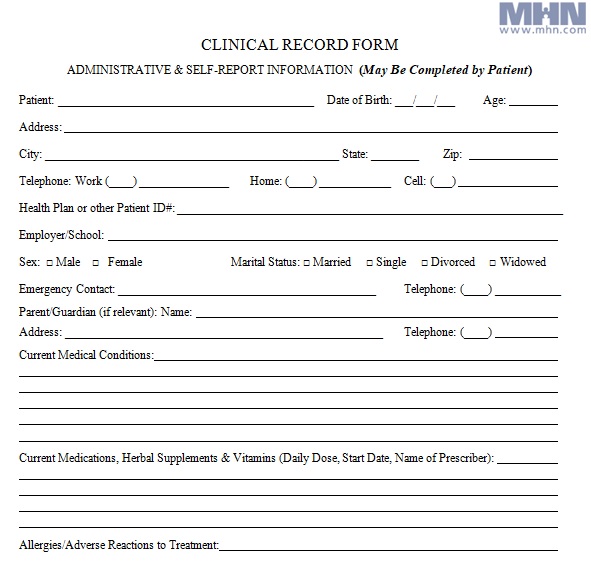
Elements of Progress Note Template
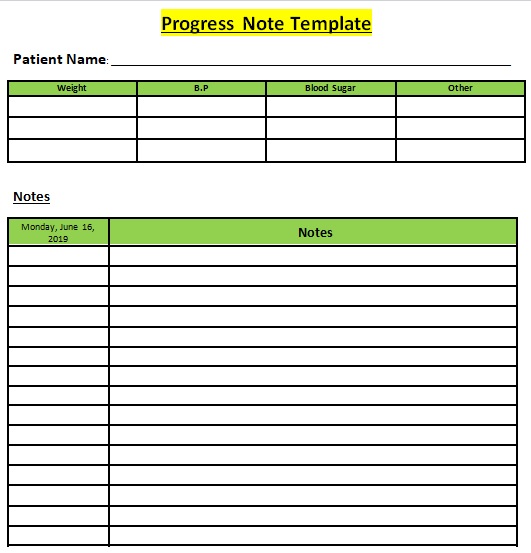
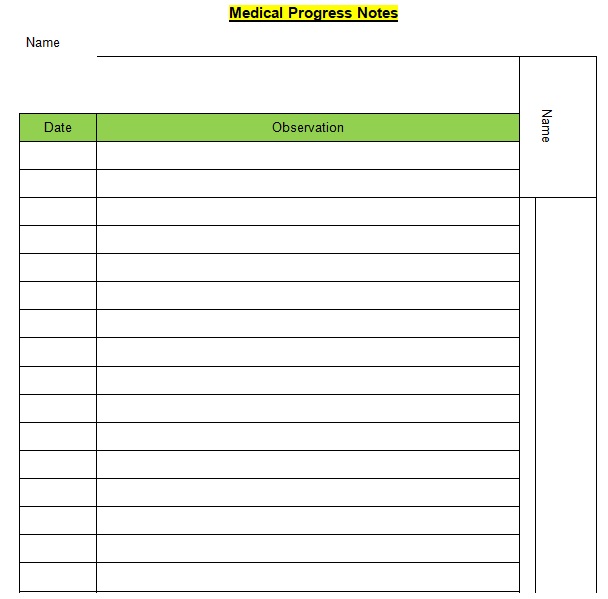
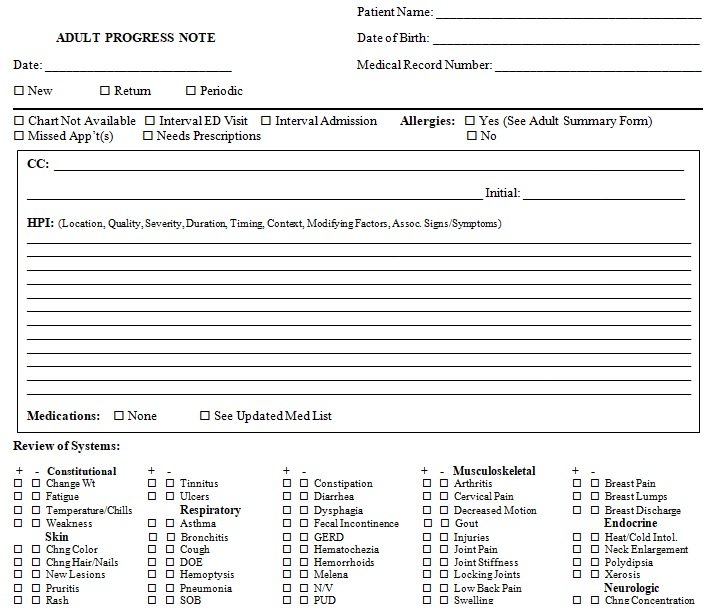
There are several components of the progress note template. It depends on the information required to be recorded by the health professional. The following details must be included in the progress note template:
- Name of the Patient
- Date of Birth
- Patient No.
- Name of the Doctor
- Diagnosis
- Symptoms
- Date
- Progress Notes
- Next Appointment
- Review Date
- Treatment Plan
- Signature and Date
How Should I Write a Progress Note?
Here are some important elements that you should keep in view while writing a progress note. Let us discuss them one-by-one;
- Purpose/objective: Observe the facts; keep in view how it will affect the care plan of the patient involved.
- Be concise: To forward the message using fewer words.
- To the point: Get relevant quickly.
- Legible: A progress note must be well spelled, well written, and sentence structure will be fine.
- Patient Privacy: Respect patient privacy.
A health professional should use critical thinking to analyze, examine, and rebuild the situation. Contemplate that everyone has their own point of view about every situation. Listen to your patient attentively and then use your reasoning and draw conclusions based on facts. You can also give recommendations if needed.
How can I write a Good Patient Note?
Here are some tips to write a good patient note;
- Write down the patient note is legible and clear writing.
- Write down the date and time recorded, and the note signed.
- Use a black ink pen instead of whiteouts to make entries.
- Assign the last entries for continuity.
- Don’t use abbreviations until approved by the management.
- Write down the reasons for medication changes.
- Avoid too much copy-paste.
- Only record the pertinent information because irrelevant information doesn’t affect the treatment.
- Begins the patient’s history with past psychiatry or social history.
- Entries have to be written in an active voice for engaging reading.
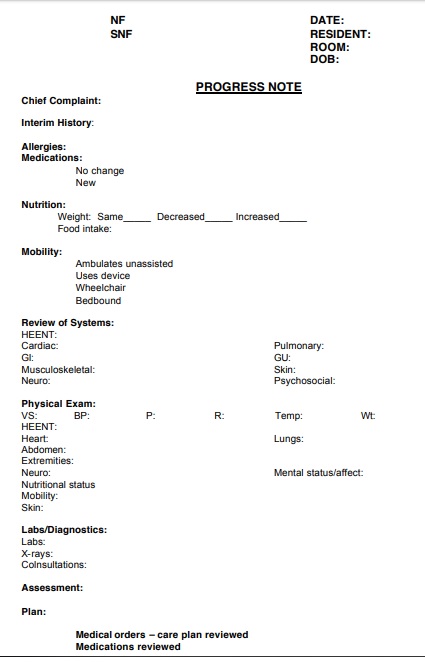
How to create effective progress notes by using the SOAP format?
Let us discuss below how each letter of the SOAP acronym can help to make an effective progress note;
S (the information given by the patient has to be recorded)
It is your responsibility as a physician or other healthcare specialist to allow your patients to inform you about all of their concerns. However, you just have to write down the things that are related to the acute medical problems like breathing problems/ improvements, new medical complaints, etc. In the S or subjective part of the progress note, don’t record the meal preferences and other irrelevant things.
O (write down the new lab results and physical exam findings)
Noting down the vital things in important like O2 saturation and daily weights. Ventilator settings, drain outputs, and fluid balance are some other pieces of information that you need to record in this section. In addition, you can also include chem sticks under labs. Here, other things to include are the physical examination of the parts related to the active medical problem (s) of the patient.
Some doctors instead of the medical problem like to examine all organs of the body. However, it isn’t necessary but there is no harm in doing this. The other important things to include here are blood tests, ECGs, x-rays, and other physical examinations.
A (specify what the patient is suffering from whether it is stationary, worsening, or improving)
There is no need to diagnose the condition again if it was already documented. After diagnosing the condition and knowing what is the issue with the patient, state whether the condition is stationary, worsening, or improving.
P (state plan for treating the condition)
In this section, you have to indicate the best way (s) of treating the patient’s condition. If what you are recommending or ordering isn’t obvious to the patient then you must provide a rationale.
How can you differentiate between SOAP notes and progress notes?
The SOAP note is one of the types of progress notes. Progress notes are available in multiple formats depending on the clinical condition at hand and the information that a health professional wants to record. While SOAP notes are the notes that consist of four sections including Subjective, Objective, Assessment, and Plan. Basically, a SOAP note is a progress note that has particular information in a certain format that enables the readers to gather information about every aspect of the session.
How can you differentiate between progress notes and psychotherapy notes?
Let us discuss below the difference between progress notes and psychotherapy notes;
Progress notes
Progress notes are the professional documents that deliver the patient’s treatment plan between healthcare providers. These notes can note down by any care provider involved in a treatment plan for the patient. They may include the following details;
- Medical history
- Allergies
- Prescriptions
- Past treatments
- Details of the current treatment plan
- Current condition
- Diagnoses
- Test data
Psychotherapy notes
Psychotherapy notes are also professional notes that provide insights into patients’ therapy and their treatment plan. These notes are written by psychologists, Psychiatrists, counselors, and psychotherapists. They may include information about the observations, hypotheses, feelings, or thoughts of the therapists regarding the session.
Do’s and Don’ts of Progress Note Template
There are several guidelines to carefully follow while creating a progress note template. Following are the dos and don’ts of creating a progress note:
- Be Concise
- Include All Details
- Carefully describe the Treatment
- Write legibly
- Take care of the Patient Privacy
- Document the Responses of the others
- Clearly explain the reason for disregarding consultant advice.
- Never type disrespect about a patient.
The progress note template can be created using MS excel and word for print-friendly nature and easy customization.
Faqs (Frequently Asked Questions)
These notes are issued by a doctor or nurse and they are valid for the longest time under the medical records. In short, they are valid until the patient is cured. Also, you can keep them for future reference.
You shouldn’t include unnecessary information in a progress note. You should ensure that it just includes what is relevant to the patient and his/her treatment.
There are four sections of a progress note;
1- Subjective
2- Objective
3- Assessment
4- Plan